When will we transform our deadly insurance system?
November 4, 2021
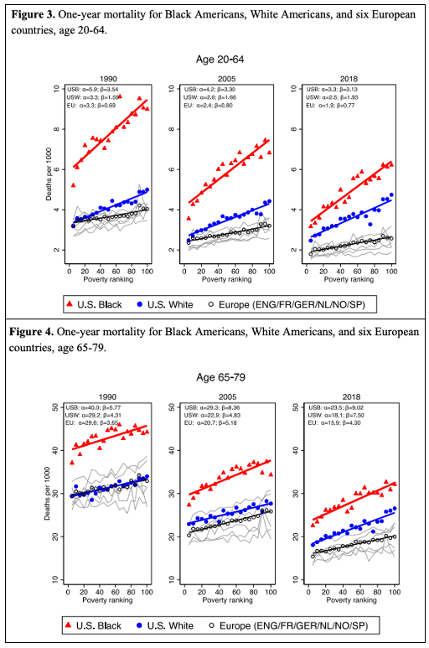
Summary: New research with vital statistics data finds that since 1990 overall US mortality has increasingly worsened compared with other OECD countries, in poorer and richer geographic areas alike. The differences attenuate after age 65, when Medicare eligibility begins. The toll for Black Americans is worse, despite gains. These findings suggest that insurance shortfalls lead to hundreds of thousands of excess deaths per year.
Inequality In Mortality Between Black and White Americans By Age, Place, and Cause, and In Comparison To Europe, 1990-2018
NBER Working Paper No. 29203
September 2021
By Hannes Schwandt et al.
From Abstract:
Inequalities in life expectancy are starker in the U.S. than in Europe. In 1990 White Americans and Europeans in rich areas had similar overall life expectancy, while life expectancy for White Americans in poor areas was lower. But since then even rich White Americans have lost ground relative to Europeans.
Life expectancy for both Black and White Americans plateaued or slightly declined after 2012, but this stalling was most evident among Black Americans even prior to the COVID-19 pandemic.
From Results:
Comment by: Jim Kahn
This excellent comprehensive research on mortality in the US vs European countries since 1990 has several compelling lessons:
1) Black American mortality still greatly exceeds White American mortality, despite a shrinking gap over 30 years.
2) Overall US mortality exceeds European country mortality by increasing margins over the last 30 years. We’re falling further behind.
3) These mortality differences are present across low to high poverty geographic areas (in the US, counties). The differences are larger in poor areas.
4) The US-Europe mortality differences are proportionally much larger age 20-64 than age 65-79 – when Medicare coverage is near universal.
5) I did a calculation. The US excess mortality age 20-64 is about 1.4 per 1000 per year. Some of that is due to non-insurance factors. If 1.0 per 1000 is attributable to insurance, applied to the 190 million in this age range, that’s 190,000 extra deaths per year.
6) However, in 2018 (after the rise of Medicare Advantage with harder to obtain care for the sick) US mortality 64-79 exceeds European levels. This suggests more insurance-related deaths.
Our insurance system is inefficient, inequitable, and deadly. Enough reason yet for radical transformation?
You might also be interested in...
Recent and Related Posts
Laying out the Ill-Effects of Medicaid Cuts in the Congressional Budget Bill
