Medicare Advantage Overpayment >$100 Billion
October 9, 2023
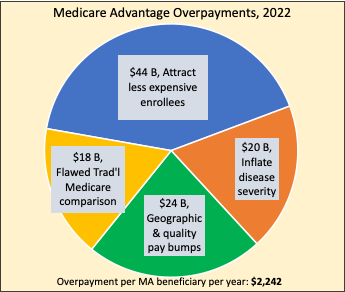
Summary: Physicians for a National Health Program released a valuable summary of Medicare Advantage overpayments. The scope and scale is breathtaking: $100 billion annual payoff for attracting inexpensive enrollees, upcoding disease severity, and biased price-setting procedures.
OUR PAYMENTS THEIR PROFITS: Quantifying Overpayments in the Medicare Advantage Program
Physicians for a National Health Program
October 2023
By our estimate, and based on 2022 spending, Medicare Advantage overcharges taxpayers by a minimum of 22% or $88 billion per year, and potentially by up to 35% or $140 billion.By comparison, Part B premiums in 2022 totaled approximately $131 billion, and overall federal spending on Part D drug benefits cost approximately $126 billion. Either of these— or other crucial aspects of Medicare and Medicaid—could be funded entirely by eliminating overcharges in the Medicare Advantage program.
[Patient Selection] results in a level of overpayment that is anywhere from 11-14%, or about $44-56 billion per year based on total MA spending for 2022.
[Diagnostic upcoding] accounted for … close to 5% of total payments … $20 billion.
Quality bonuses and county benchmarks together … constitute 6-7% in excess payments to MA, which for 2022 … amounts to $24-28 billion.
Induced utilization … results in an overpayment of approximately $36 billion
Comment by: Jim Kahn
Tracking how Medicare Advantage games the Medicare payment system isn’t easy – there are multiple components, with considerable technical complexity. PNHP has done a huge service by assembling the data in one easy-to-understand and well-cited review. The bottom line: Medicare Advantage plans take home about $100 billion annually in payments that have nothing to do with providing care. Ill-gotten gains, in my view.
Below is my summary in graphic form. I’ve picked the best number for each category, based on my assessment of the relevant analyses. The total is $106 billion, well within PNHP’s range. The bonus to MA plans, even after allowing that some of this money adds to MA benefits, is about $2,242 per enrollee per year.
Here’s a quick key:
Attract less expensive enrollees (in technical jargon, “Risk selection”) means finding and keeping MA beneficiaries who use less medical care even when adjusted for their disease severity scores. The MedPAC analysis cited in the PNHP report is particularly compelling.
Inflate disease severity (“upcoding”) means assigning beneficiaries disease severity scores that are above those used in traditional Medicare (TM), and often fraudulent. The $20 billion estimate may be conservative.
Flawed Traditional Medicare comparison (aka “Induced utilization”) is a technical issue with how TM costs are used to set MA benchmarks. In brief, with widespread use of MediGap plans, TM medical care use rises, and MA plans get the benefit of that bump despite imposing more financial barriers to care.
Geographic & quality pay bumps are supplements to reimbursement rates beyond the values based on TM spending. Quality ratings are gamed to get perfect scores, and have little if anything to do with clinical outcomes.
Why are we plowing through these tricky numbers? Because MA plans are grabbing huge piles of money that comes from taxpayers and Medicare enrollees.
These problems disappear under single payer. The money we spend on health care will go to … health care.
About the Commentator, Jim Kahn
Jim (James G.) Kahn, MD, MPH (editor) is an Emeritus Professor of Health Policy, Epidemiology, and Global Health at the University of California, San Francisco. His work focuses on the cost and effectiveness of prevention and treatment interventions in low and middle income countries, and on single payer economics in the U.S. He has studied, advocated, and educated on single payer since the 1994 campaign for Prop 186 in California, including two years as chair of Physicians for a National Health Program California.
See All PostsYou might also be interested in...
Recent and Related Posts
Premier Medical Journal Scrutinizes Corporatization of US Health Care
Laying out the Ill-Effects of Medicaid Cuts in the Congressional Budget Bill
