Incredible (Terrible) Shrinking Physician Supply
Waiting times for physician appointments are growing. The immediate cause is contraction of the physician workforce. The root cause is clinician burnout, in large part due to fragmented insurance and resulting make-work inefficiencies. Single payer will help.
September 7, 2024
Health shrinkflation: Patients wait more for less
Axios
Sep 3, 2024
By Tina Reed
The U.S. spends more on health care than almost anywhere else. But increasingly patients are getting less in return, and enduring long waits to get not as much face-time with their clinician.
Why it matters: Shrinkflation is hitting a sector that accounts for almost one-fifth of the economy, eroding the doctor-patient relationship and leaving many turning to urgent care clinics or telehealth services.
> Some who can afford it are gravitating to concierge practices that offer fewer hoop jumps and more add-on services with office visits.
The latest: The trend is being felt especially in primary care, but also in many specialties.
> An Axios-Ipsos survey last month found that nearly one in five respondents said they had to wait more than two months to see a primary care physician or specialist, with waits trending longest in the Midwest.
> NYC Health + Hospitals recently told primary care doctors to cut appointment times in half to 20 minutes, in order to squeeze in more patients, Gothamist reported.
> A spokesperson told Axios that the public health system is grappling with 50,000 more primary care patients who’ve been added since 2021. The average number of days to the third next available appointment jumped from 12 days to 22 days.
By the numbers: 17% of patients had to wait one to three months for their latest doctor’s appointment, per electronic health records company Tebra.
> The most frequently cited specialties with long wait times included neurology (26%), ear, nose, and throat (26%), psychiatry (20%), and OB/GYN (17%). Primary care stood at 19%.
> 43% of patients reported experiencing longer wait times for appointments since the pandemic, per the Tebra survey.
> The surge in demand for in-person care since the crisis has been well-documented. AMN/Merritt Hawkins found that the average wait time for a physician appointment in 15 large metro markets surveyed in 2022 was 26 days, up from roughly 24 days in 2017, and about 21 days in 2004.
The big picture: This is what shrinkflation in healthcare looks like as the industry struggles with supply and demand issues, Robert Pearl, a Stanford University professor and former CEO of The Permanente Medical Group, told Axios.
> There’s been across-the-board growth in patient volumes largely from pent-up demand for services many put off during the pandemic.
> At the same time, tens of thousands of doctors have left the field due to burnout and other factors, and surveys indicate even more plan to retire early.
> Red tape around insurance and rising out-of-pocket costs are leaving patients frustrated and confused, and in some cases burdened by more medical debt.
“You’re paying actually more for your health coverage, but you’re not getting more. You’re actually getting less,” Pearl said.
Comment by: Jim Kahn
The physician supply is steadily contracting, especially in primary care. This lengthens waits for clinical visits, not to mention the challenge of finding a new provider. Each year we pay more in premiums and cost-sharing, yet we suffer increasing challenges getting the care we need.
What’s going on? This tightening of physician supply reflects some simple math: more individuals leave clinical medicine than new trainees enter. Increasing the number of mid-level providers, like nurse practitioners, is a viable and valuable option. However, the physician flow dynamics remain critical. And recent trends are not encouraging:
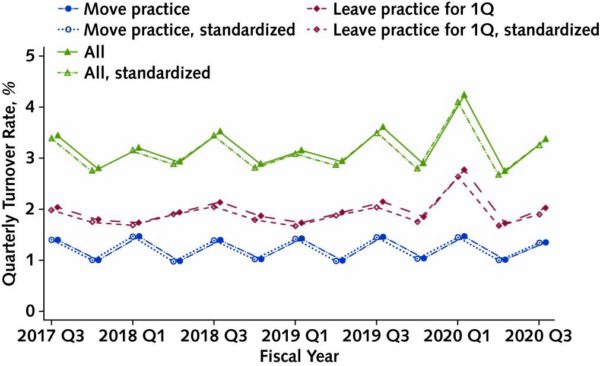
This is ongoing: 7% of physicians left the workforce in 2021 and 2022. Nearly 1 in 4 physicians stated an intention to leave practice within two years. Long-term projections for physician supply are dire.
Why are so many doctors leaving? The short answer is growing burnout:
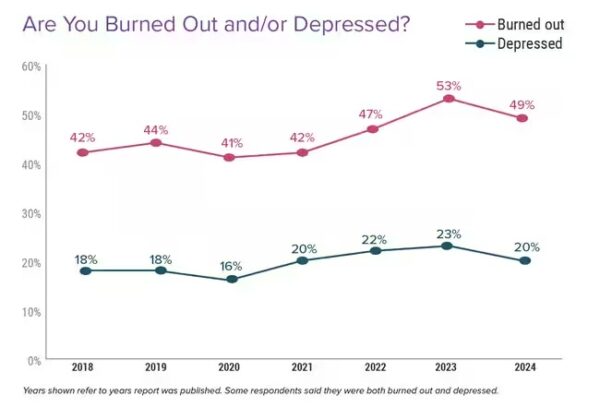
And why the burnout?
Too many bureaucratic tasks (eg, charting, paperwork): 62%
Too many hours at work: 41%
Lack of respect from administrators / employers, colleagues, staff: 40%
Insufficient compensation: 38%
Lack of control / autonomy: 32%
(full list here)
All of these causes reflect, in substantial degree, our fragmented insurance system and the central role of for-profit insurers and provider groups. Here’s how single payer would help with each:
* Reduce bureaucracy: eliminate an hour/day of billing & insurance-related tasks done by physicians.
* Reduce hours at work: less time on bureaucracy; more providers especially in primary care.
* Build respect: bolster the clinical role of physicians, and foster clinician-run practices.
* Correct compensation inequities: Increase payment rates for primary care.
* Build autonomy: make clinician-run practices more financially and administratively viable.
Single payer isn’t a magic potion for physician emotional well-being. But it is a viable framework to build clinical focus and autonomy, and to foster equity among specialties (and of course among populations groups). It is the only way to break out of our burnout quagmire.
About the Commentator, Jim Kahn
Jim (James G.) Kahn, MD, MPH (editor) is an Emeritus Professor of Health Policy, Epidemiology, and Global Health at the University of California, San Francisco. His work focuses on the cost and effectiveness of prevention and treatment interventions in low and middle income countries, and on single payer economics in the U.S. He has studied, advocated, and educated on single payer since the 1994 campaign for Prop 186 in California, including two years as chair of Physicians for a National Health Program California.
See All PostsYou might also be interested in...
Recent and Related Posts
Saturday! National Day of Action for Single Payer
GOP Medicaid Cuts: Multifaceted, Severe, Deadly, Machiavellian
